ITUP Blog: 2025-26 Introduced Bills
By Shirley Lam, MPH
2025-26 Introduced Bills
Overview: The deadline for introducing legislation for the first year of the 2025-2026 legislative session was February 21, 2025. Legislation introduced this year focuses on improving access to equitable and affordable health care, transforming the health care delivery system with a focus on reproductive, perinatal, behavioral health care, and the future of health with technological innovations.
Summary and Policy Areas: This blog summarizes introduced legislation that proposes solutions relating to ITUP’s three priority policy issues: health care coverage and access, delivery system transformation, and the future of health.
Additionally, we noted with icons which bills address:
- Health Equity
- Behavioral & Mental Health
- Delivery System Transformation
- Consumer Protections
- Artificial Intelligence (AI)
Legislative Bill Process Guide: At the end of this blog, we also include important information on the legislative bill process, helpful links, and a timeline with dates that can be used to follow these bills throughout the years.
Note: This is not a comprehensive list of all the health and health care-related bills that were introduced. If you have questions about a bill not listed here, please feel free to contact us at info@itup.org
Additionally, we noted with icons which bills address:
Health Care Coverage and Access:
Health Care Coverage Essential Health Benefits: AB 224 (Bonta) and SB 62 (Menjivar) aim to have the Legislature review and update the list of essential health![]() benefits and create a new benchmark plan starting in 2027. AB 224 and SB 62 limit the applicability of the current benchmark plan to health plans until 2027.
benefits and create a new benchmark plan starting in 2027. AB 224 and SB 62 limit the applicability of the current benchmark plan to health plans until 2027.
Health Care Coverage Cost Sharing: AB 298 (Bonta) prohibits health care plans and disability insurance policies from charging out-of-pocket expenses like deductibles,![]() copayments, or coinsurance for services provided to Californians under 21 years old, starting January 1, 2026. AB 298 prohibits individuals or companies from charging or seeking payment for services given to patients under 21 years of age; if a health care plan breaks this rule, it could be treated as a crime.
copayments, or coinsurance for services provided to Californians under 21 years old, starting January 1, 2026. AB 298 prohibits individuals or companies from charging or seeking payment for services given to patients under 21 years of age; if a health care plan breaks this rule, it could be treated as a crime.
Covered California Expansion: AB 4 (Arambula) expands access to Covered California by allowing all Californians, regardless of immigration status, to purchase health insurance through the marketplace. AB 4 requires Covered California to execute a mirror exchange program on its own to expand coverage to ![]() undocumented people under existing federal rules and subsidies if they are available. In addition, AB 4 requires Covered California to promote the program and help Californians get enrolled beginning October 1, 2028, and creates the Covered California for All Fund to manage money from fees, appropriations, and other sources to fund the program. See ITUP’s Issue Brief on Expanding Health Coverage for California Farmworkers for more details on the impact of AB 4.
undocumented people under existing federal rules and subsidies if they are available. In addition, AB 4 requires Covered California to promote the program and help Californians get enrolled beginning October 1, 2028, and creates the Covered California for All Fund to manage money from fees, appropriations, and other sources to fund the program. See ITUP’s Issue Brief on Expanding Health Coverage for California Farmworkers for more details on the impact of AB 4.
Health Care Delivery System Transformation:
Medi-Cal Home and Community-Based Alternatives (HCBA) Waiver: AB 315 (Bonta) removes the rule in the HCBA Waiver that allows adding up to 5,000 more slots for the waiver and instead requires enrollment of all eligible individuals who applied for the HCBA Waiver. AB 315 requires the Department of Health Care Services (DHCS) to submit a report by March 1, 2026, examining how well the current rates for the waiver program work, including an evaluation of how the services are being paid for, and to consider sustainability and effectiveness factors.
Medi-Cal Adverse Childhood Experiences (ACEs) Trauma Screenings Providers: AB 29 (Arambula) requires DHCS to allow community-based organizations, local![]()
![]() health groups that use community health workers (CHWs), and doulas to provide ACES trauma screenings if they are enrolled Medi-Cal providers. These providers will also be eligible to be paid for offering such screenings. In addition, AB 29 requires DHCS to make changes to state plans and seek any federal approvals necessary to implement these services. AB 29 requires DHCS to update its website and the ACEs Aware website to reflect the addition of new Medi-Cal providers now authorized to provide ACEs screenings.
health groups that use community health workers (CHWs), and doulas to provide ACES trauma screenings if they are enrolled Medi-Cal providers. These providers will also be eligible to be paid for offering such screenings. In addition, AB 29 requires DHCS to make changes to state plans and seek any federal approvals necessary to implement these services. AB 29 requires DHCS to update its website and the ACEs Aware website to reflect the addition of new Medi-Cal providers now authorized to provide ACEs screenings.
Homeless Pupils California Success, Opportunity, and Academic Resilience (SOAR) Guaranteed Income Program: SB 33 (Cortese) establishes a statewide guaranteed income pilot program titled the California SOAR Guaranteed Income Program. SB 33 aims to provide students experiencing homelessness with direct cash assistance to support their transition out of high school and their access to employment and post-secondary education.
Medi-Cal Street Medicine: AB 543 (González) introduces and integrates street medicine into Medi-Cal , complementing existing programs like CHWs, enhanced care management (ECM) and Community Supports (CS) to provide health services directly to unhoused Californians. In addition, AB 543 allows unhoused Californians![]() to automatically qualify for full-scope Medi-Cal benefits during the eligibility process. In addition, unhoused individuals will have access to any Medi-Cal provider, with Medi-Cal managed care plans (MCPs) covering costs and setting reasonable rules aligned with service areas. AB 543 requires MCPs to allow members to report whether they are experiencing homelessness online, in person, or by phone. In addition, DHCS is required to inform MCPs if a member has indicated they are experiencing homelessness based on their Medi-Cal application. AB 543 requires DHCS to ensure the Medi-Cal program and the California Statewide Automated Welfare System (CalSAWS) mutually share information about Californians applying for or receiving Medi-Cal who are experiencing homelessness but will ensure privacy protections are in place.
to automatically qualify for full-scope Medi-Cal benefits during the eligibility process. In addition, unhoused individuals will have access to any Medi-Cal provider, with Medi-Cal managed care plans (MCPs) covering costs and setting reasonable rules aligned with service areas. AB 543 requires MCPs to allow members to report whether they are experiencing homelessness online, in person, or by phone. In addition, DHCS is required to inform MCPs if a member has indicated they are experiencing homelessness based on their Medi-Cal application. AB 543 requires DHCS to ensure the Medi-Cal program and the California Statewide Automated Welfare System (CalSAWS) mutually share information about Californians applying for or receiving Medi-Cal who are experiencing homelessness but will ensure privacy protections are in place.
Medi-Cal Enhanced Care Management and Community Supports: SB 324 (Menjivar) requires Medi-Cal MCPs that offer ECM or CS services to prioritize working with local community providers, as long as those providers are available in the area and have experience in offering ECM or CS services. In addition, SB 324![]() mandates ECM and CS providers to be involved in the planning process and requires DHCS to create simple, standardized forms for MCPs to use and give instructions on how local providers can work together by subcontracting with one another. SB 324 requires DHCS to annually update payment guidelines for MCPs to reimburse for ECM and CS services.
mandates ECM and CS providers to be involved in the planning process and requires DHCS to create simple, standardized forms for MCPs to use and give instructions on how local providers can work together by subcontracting with one another. SB 324 requires DHCS to annually update payment guidelines for MCPs to reimburse for ECM and CS services.
Workforce
Residential Care Facilities for the Elderly – Direct Care Ratios: AB 508 (Aguiar-Curry) requires residential care facilities for the elderly (RCFEs) to calculate and keep records of how many caregivers are available for residents and to keep those records for a minimum of 12 months. In addition, AB 508 requires RCFEs to disclose these ratios with residents or their representatives upon move in or any time there is a price increase. AB 508 requires each RCFE to make the direct care ratio publicly accessible on their websites and in common areas like lunchrooms or lobbies. In addition, the website and promotional materials must clearly explain that the ratios are calculated daily and are available for anyone to request, covering the past 12 months.
Workforce Development Poverty-Reducing Labor Standards: Funds, Programs, Reporting and Analyses: SB 21 (Durazo) creates the Equity, Climate Resilience, and Quality Jobs Fund and requires 1% of federal money to be transferred into this fund. In addition, SB 21 states that these funds would be used to support workforce programs that meet certain labor standards aimed at reducing poverty, ensuring fair wages, and encouraging climate resilience. SB 21 requires all state agencies administering these funds to develop and adopt poverty-reducing labor standards and to generate reports on the progress. In addition, SB 21 requires the California Workforce Development Board to contract with a research institution to analyze how well these programs are creating fair, sustainable jobs and helping the environment.
Mental Health Black Mental Health Navigator Certification: AB 73 (Jackson) requires the California Department of Health Care Access and Information (HCAI)![]()
![]() to create a special certification program and training for Black Mental Health Navigators to help guide and support individuals in accessing mental health services in Black communities. In addition, AB 73 requires HCAI to track and publish data annually on the number of people certified through this program and how many are working in community health roles. See ITUP’s Fact Sheet California Health Care Specialty Workforce Shortages for more information.
to create a special certification program and training for Black Mental Health Navigators to help guide and support individuals in accessing mental health services in Black communities. In addition, AB 73 requires HCAI to track and publish data annually on the number of people certified through this program and how many are working in community health roles. See ITUP’s Fact Sheet California Health Care Specialty Workforce Shortages for more information.
Community Health Workers: AB 96 (Jackson) expands the definition of CHWs to include peer support specialists, who are people with personal experience![]() with a particular health issue and help others going through the same thing. In addition, AB 96 states that if a peer support specialist is certified, they will be considered to have completed all the education and training needed to be certified as a CHW. ITUP’s Fact Sheet Community Health Workers and the Health Care Delivery System to learn more about the integral role CHWs play in closing equity gaps for the health of Californians.
with a particular health issue and help others going through the same thing. In addition, AB 96 states that if a peer support specialist is certified, they will be considered to have completed all the education and training needed to be certified as a CHW. ITUP’s Fact Sheet Community Health Workers and the Health Care Delivery System to learn more about the integral role CHWs play in closing equity gaps for the health of Californians.
Medi-Cal Community Health Worker Services: AB 403 (Carrillo) requires DHCS to annually review outreach and education efforts conducted by Medi-Cal MCPs![]() and conduct an annual analysis of the CHW services benefit beginning July 1, 2027, of how CHW services are being utilized by Medi-Cal members. The analysis will include data on how many CHWs are available, what the needs of Medi-Cal members are, disaggregation of information by location, race, ethnicity, language, age, etc., and include data on how much Medi-Cal pays for the CHWs benefit.
and conduct an annual analysis of the CHW services benefit beginning July 1, 2027, of how CHW services are being utilized by Medi-Cal members. The analysis will include data on how many CHWs are available, what the needs of Medi-Cal members are, disaggregation of information by location, race, ethnicity, language, age, etc., and include data on how much Medi-Cal pays for the CHWs benefit.
Mental Health and Substance Use Disorders (SUDs)
Health Care Coverage and Mental Health and Substance Use Disorders Inpatient Admissions: AB 384 (Connolly) prohibits health insurance plans, beginning![]() on January 1, 2027, from requiring prior authorization before admitting someone to a hospital for a mental health or substance use disorder (SUD) treatment, as long as it’s medically necessary. In addition, AB 384 states that no approval will be needed for any necessary health care services given while the person is in the hospital. AB 384 prohibits the requirement of prior authorization for Medi-Cal members for medically necessary admission to a hospital for 24-hour care for mental health or SUD treatment.
on January 1, 2027, from requiring prior authorization before admitting someone to a hospital for a mental health or substance use disorder (SUD) treatment, as long as it’s medically necessary. In addition, AB 384 states that no approval will be needed for any necessary health care services given while the person is in the hospital. AB 384 prohibits the requirement of prior authorization for Medi-Cal members for medically necessary admission to a hospital for 24-hour care for mental health or SUD treatment.
Alcohol and Drug Recovery or Treatment Facilities Discharge and Continuing Care Planning: AB 423 (Davies) requires DHCS to create rules that require alcohol![]()
![]() and drug recovery or treatment facilities to ensure patients have a continuous care plan following discharge. This includes helping patients return to their community after treatment and ensuring they have a scheduled follow-up appointment with a mental health or substance use professional within seven days following discharge.
and drug recovery or treatment facilities to ensure patients have a continuous care plan following discharge. This includes helping patients return to their community after treatment and ensuring they have a scheduled follow-up appointment with a mental health or substance use professional within seven days following discharge.
Veterans Mental Health: AB 81 (Ta) requires the Department of Veterans Affairs (VA) to create a program to fund a study on mental health issues among women![]() veterans in California. In addition, AB 81 requires the VA to submit a report to the Legislature with the study’s findings and recommendations by June 30, 2029. These requirements will sunset on January 1, 2030. See ITUP’s Policy Toolkit Behavioral Health in California for more information.
veterans in California. In addition, AB 81 requires the VA to submit a report to the Legislature with the study’s findings and recommendations by June 30, 2029. These requirements will sunset on January 1, 2030. See ITUP’s Policy Toolkit Behavioral Health in California for more information.
Future of Health
Artificial Intelligence (AI)
Health Care Professions Deceptive Terms or Letters Artificial Intelligence: AB 489 (Bonta) prohibits the use of specified terms, letters, or phrases in AI technology![]() that suggests it has a health care license or certification, especially if the AI is being used to give medical advice or information. In addition, if AI is used to communicate patient information, it must also include a clear disclaimer that the communication was generated by AI and provide instructions on how to contact a real health care provider. See ITUP’s Fact Sheet Catalyzing AI to Advance Health Equity in California Communities and ITUP’s Policy Toolkit The Emergence of Artificial Intelligence and It’s Application in Health for more information about the impact of AI in health care.
that suggests it has a health care license or certification, especially if the AI is being used to give medical advice or information. In addition, if AI is used to communicate patient information, it must also include a clear disclaimer that the communication was generated by AI and provide instructions on how to contact a real health care provider. See ITUP’s Fact Sheet Catalyzing AI to Advance Health Equity in California Communities and ITUP’s Policy Toolkit The Emergence of Artificial Intelligence and It’s Application in Health for more information about the impact of AI in health care.
Broadband & Telehealth
Communications Broadband Internet Service Providers Affordable Home Internet: AB 353 (Boerner) requires internet service providers (ISPs) to offer affordable home internet to people living in California. ITUP’s Issue Brief Addressing Digital Equity for Equitable, Accessible Health Care and ITUP’s Fact Sheet Snapshot: Addressing Digital Equity for Equitable and Accessible Health Care for more information on the role that broadband access plays in the health of Californians.
Telehealth for All Act of 2025: AB 688 (González) requires DHCS to publish a report every 2 years, beginning in 2028, that analyzes how telehealth is being used in the Medi-Cal program. The report will utilize Medi-Cal data to look at how telehealth is helping people get care, the quality of care, and the costs, while also disaggregating the data based on location, race, and social determinants of health (SDoH) categories to identify disparities in accessibility of telehealth services. In addition, AB 688 requires DHCS to identify additional data elements to better understand and improve access to telehealth for everyone. See ITUP’s Fact Sheet Telehealth and COVID-19 to learn more about telehealth policies that were put into place during the public health emergency.
Specialty Care Network Telehealth and Other Virtual Services: AB 257 (Flora) requires the California Health and Human Services Agency (CalHHS), in![]() collaboration with HCAI and DHCS to establish a demonstration project for a telehealth and other virtual services specialty care network that is designed to serve patients of safety-net providers consisting of qualifying providers, defined to include, among others, rural health clinics and community health centers.
collaboration with HCAI and DHCS to establish a demonstration project for a telehealth and other virtual services specialty care network that is designed to serve patients of safety-net providers consisting of qualifying providers, defined to include, among others, rural health clinics and community health centers.
Privacy Protection & Data Sharing
California Health and Human Services Data Exchange Framework: SB 660 (Menjivar) requires, by January 1, 2026, with designated funds in the state budget, the Center for Data Insights and Innovation (CDII) to manage and expand the CalHHS Data Exchange Framework (DxF) to share important health and social services data between various organizations. SB 660 expands the mandated entities required to sign the data sharing agreement (DSA) and authorizes CDII to decide which additional organizations will be required to join. In addition, SB 660 requires CDII to establish a process by July 1, 2025, to designate qualified health information organizations (QHIOs) as data-sharing intermediaries. SB 660 requires CDII to publish an annual report to the Legislature, including compliance with data sharing agreements. In addition, SB 660 expands membership of the stakeholder advisory group that helps guide the program and creates a CalHHS Data Exchange Board, composed of 12 members who will review and approve changes to the data sharing rules and agreements. See ITUP’s Issue Brief Leveraging Data to Advance Health Equity and Success in CalAIM, ITUP’s Fact Sheet California Data Exchange Framework 101, and complimentary Policy Toolkit for more information.
Medi-Cal Behavioral Health Data Sharing: AB 618 (Krell) requires each Medi-Cal MCPs, county specialty mental health plan, Drug Medi-Cal certified program, and the Drug Medi-Cal organized delivery system (DMC-ODS) program, to electronically share data to improve patient care. The data shared will help track and support the care of individuals. In addition, AB 618 requires DHCS to determine minimum data elements and the frequency and format of data sharing through a stakeholder process and guidance, with final guidance published by January 1, 2027.
Health Facilities Information Sharing: SB 81 (Arreguin) states the intent of the Legislature to prohibit health care facilities from working with immigration![]() authorities or sharing patient information, including medical records, with them.
authorities or sharing patient information, including medical records, with them.
Privacy Health Care Data: AB 45 (Bauer-Kahan) aims to make it illegal to use geofencing (tracking a specific location) around health care places that![]() provide in-person services, like clinics. In addition, it would also stop health care providers from sharing medical research or information about someone seeking an abortion if it’s requested by another state that has laws that interfere with a person’s right to privacy under the Reproductive Privacy Act.
provide in-person services, like clinics. In addition, it would also stop health care providers from sharing medical research or information about someone seeking an abortion if it’s requested by another state that has laws that interfere with a person’s right to privacy under the Reproductive Privacy Act.
What’s Next: Legislative Process Information
Here is a timeline with key events and deadlines that are useful for tracking legislation.
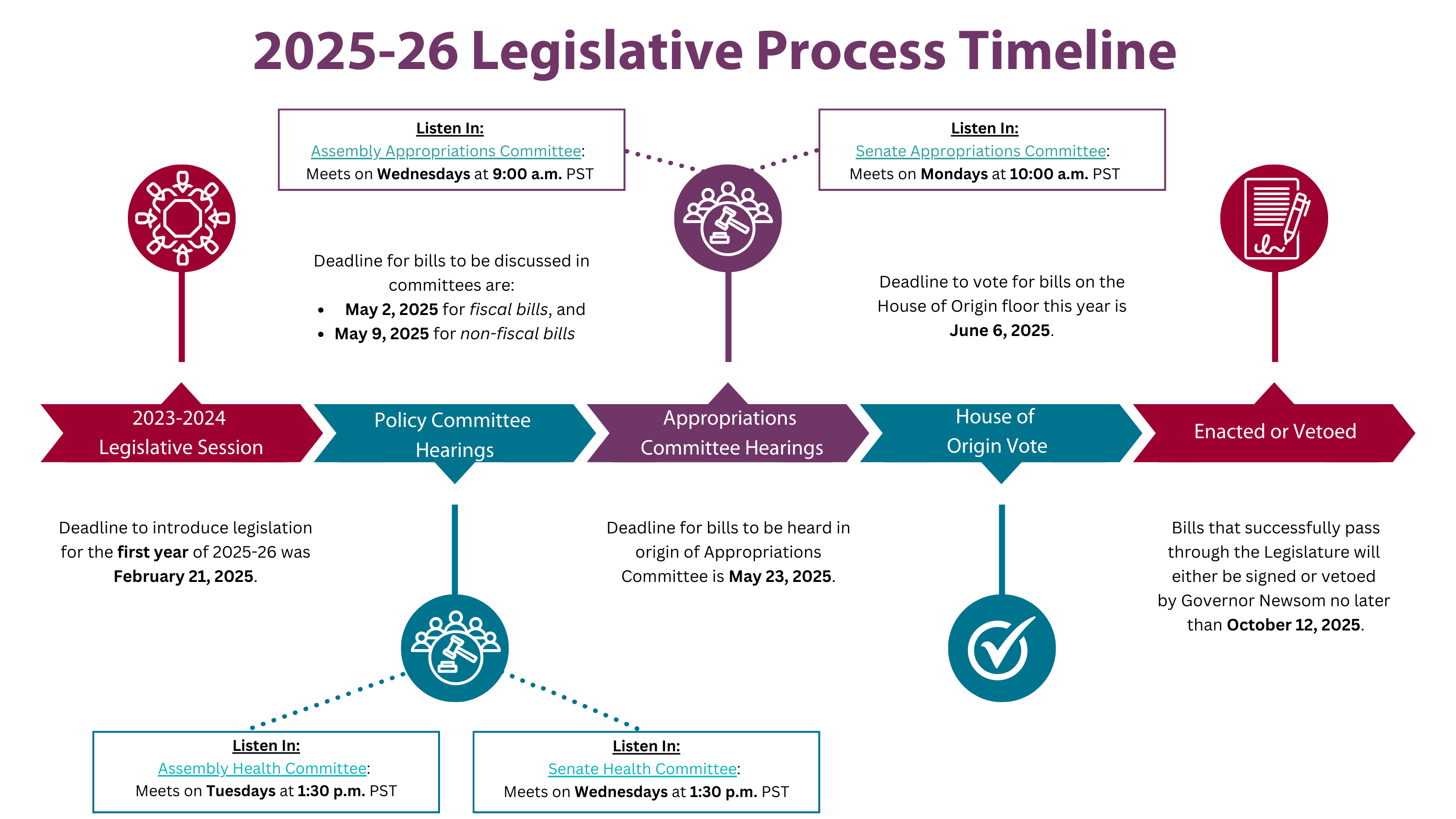
Below, we provide a detailed explanation of the timeline above and the California legislative process. The 2025 Legislative calendars for the California Assembly, and Senate include all deadlines that must be met for bills to be signed into law. The ‘house of origin’ or the ‘first house’ is the branch of the Legislature where the bill was introduced (ABs = Assembly Bills, the Assembly is the first house the bill must pass through; SBs = Senate Bills, the Senate is the first house the bill must pass through). Bills can be amended throughout the process.
Committee Hearings
Policy committees begin hearing bills in March 2025. The committees are made up of a subset of assemblymembers or senators to hear bills on a specific policy topic, such as health. The committee chairs set bills for hearing dates throughout March and April, and public hearings are recorded and can be watched live, typically in person, but live stream video is available and was preferred during the public health emergency. Assembly and Senate Health Committee hearing dates, agendas that list the bills being heard, and a link to where you, the public, can watch the hearings are found on each policy committee’s website. The deadline for bills to be discussed in committees is May 2, 2025, for fiscal bills (legislation that has a cost to the state), and May 9, 2025, for non-fiscal bills.
- Assembly Health Committee: Meets on Tuesdays at 1:30 p.m. PST
- Senate Health Committee: Meets on Wednesdays at 1:30 p.m. PST
Appropriations Committee Hearings
Once a bill passes in policy committee(s), the next step in the legislative process for most bills is a hearing in the Appropriations Committee. The Appropriations Committee reviews all bills that have a designated fiscal impact, and the deadline for bills to be heard in the house of origin appropriations committee is May 23, 2025. At this point in the Legislative process, many bills will be ‘held on suspense,’ which effectively means they will not move forward in the process. In the Assembly, any bill that has an annual cost of $150,000 or more, from any fund, gets placed on the suspense file. In the Senate, legislation with an annual cost of $50,000 General Fund or $150,000 federal funds or special funds, gets placed on the suspense file. Like the policy committees, the Appropriations Committees hold public hearings. Most bills get placed on the suspense file and are heard in committee close to the May 23, 2025, deadline.
- Assembly Appropriations Committee: Meets on Wednesdays at 9:00 a.m. PST
- Senate Appropriations Committee: Meets on Mondays at 10:00 a.m. PST
House of Origin Floor Vote
The last stop for a bill before the opposite house begins to weigh in on the policy is the ‘floor vote’. This is where all Assemblymembers vote on AB bills and all Senators vote on SB bills. The deadline for bills to be voted on the house of origin floor this year is June 6, 2025.
Following a bill’s successful passage out of its house of origin, the entire process listed above is repeated in the opposite house (Ex. Abs will then go through the Legislative process in the Senate). The last day of this year’s legislative session, and subsequently, the last day a bill can pass through the entire process, is September 12, 2025. Bills that successfully pass through the Legislature will either be signed or vetoed by Governor Newsom no later than October 12, 2025.